Cardiac Arrest - Pediatric
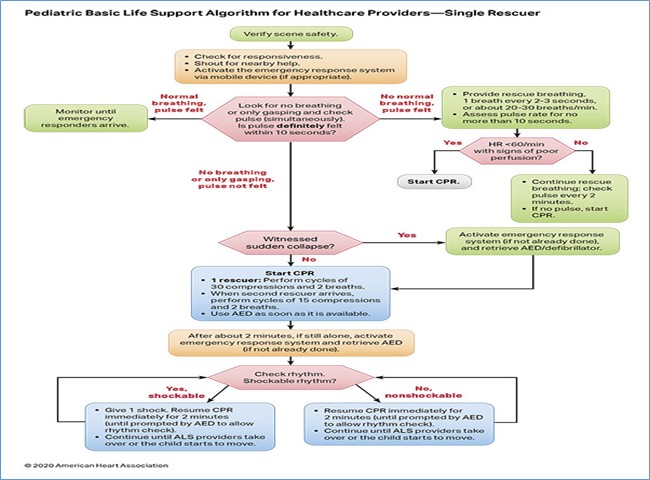
EMT STANDING ORDERS
- Routine Patient Care.
- Follow BLS guidelines as trained and credentialed.
- Check responsiveness.
- Call for advance team.
- Check patient breathing and pulse (for at least 5 but no more than 10 seconds), check breathing and pulse simultaneously.
- Performs high quality chest compression (CPR) and rescue breath (30 compressions: 2 rescue breath). During 2-rescue CPR delivers (15 compressions: 2 rescue breath).
- Apply AED and analyze the rhythm ASAP. Follow AED protocol.
- Continue CPR and AED cycles until advance unite arrive or pulse present.
- Call for AEMT/Paramedic intercept. & Assisst AEMT/Parmedic in patient care.
Note: Push hard and Push fast, Minimize Interruption for less than 10 seconds.
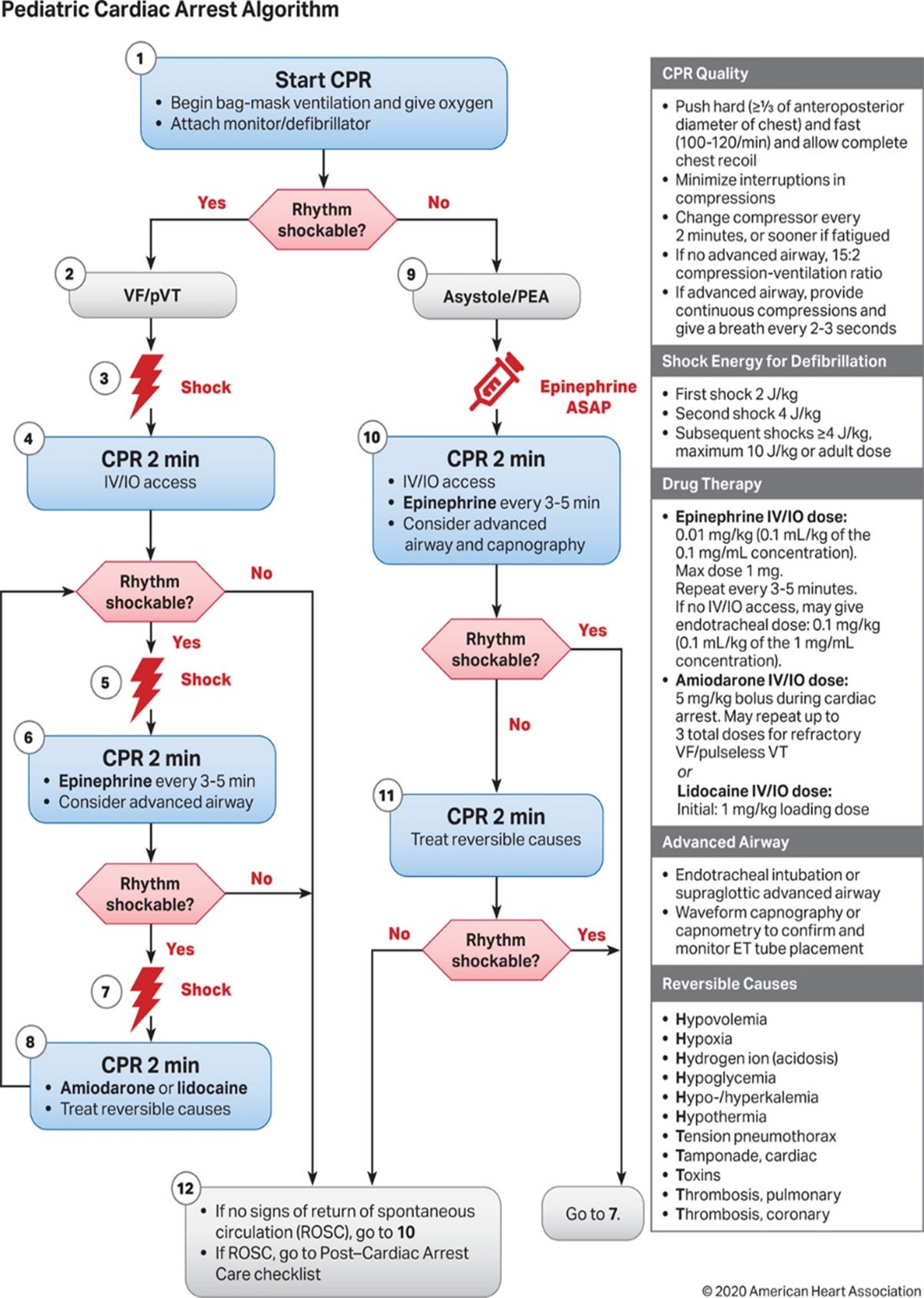
VF/Pulseless VT
AEMT/PARAMEDIC STANDING ORDERS
- Follow PALS guidelines as trained and credentialed.
- Defibrillation when available, with minimum interruption in chest compressions. Resume CPR for 2 minutes; then rhythm check, if there is no pulse; start defibrillation. Use manufacturer’s recommendations. (First shock 2 J/kg, second 4 J/kg at max dose 10 J/kg, or adult dose).
- If no response after second defibrillation and along with CPR:
- Administer Epinephrine 0.01 mg/kg ASAP (0.1 ml/kg of the 0.1mg/ml concentration, max dose 1mg) IV/IO; repeat every 3-5 minutes.
- Amiodarone 5 mg/kg, IV/IO, repeated up to 3 total doses for refractory VF/pulseless VT OR Lidocaine 1 mg/kg IV/IO.
- Consider advanced airway only if airway patency cannot be maintained using basic maneuvers and adjuncts.
- Consider and treat reversible causes. (Page 3 cardiac).
PEA / Asystole
AEMT / PARAMEDIC STANDING ORDERS
- Confirm PEA/Asystole.
- Administer Epinephrine 0.01 mg/kg ASAP (0.1 ml/kg of the 0.1mg/ml concentration, max dose 1mg) IV/IO; repeat every 3-5 minutes.
- Continue CPR and rescue breaths.
- Consider advance airway, capnography, confirm tube placement as per protocol.
- Consider and treat reversible causes. (Page 3 cardiac).
- In PEA: Check pulse every 2 minutes.