Hyperthermia (Environmental) - Adult & Pediatric
Consider hypothermia if patient has a history of cold exposure or a disease that predisposes them to hypothermia, patient’s trunk feels cold on examination, or core temperature is < 35°C (95°F).
EMT Standing Order (ADULT & PEDIATRIC)
- Routine Patient Care. Ensure scene safety.
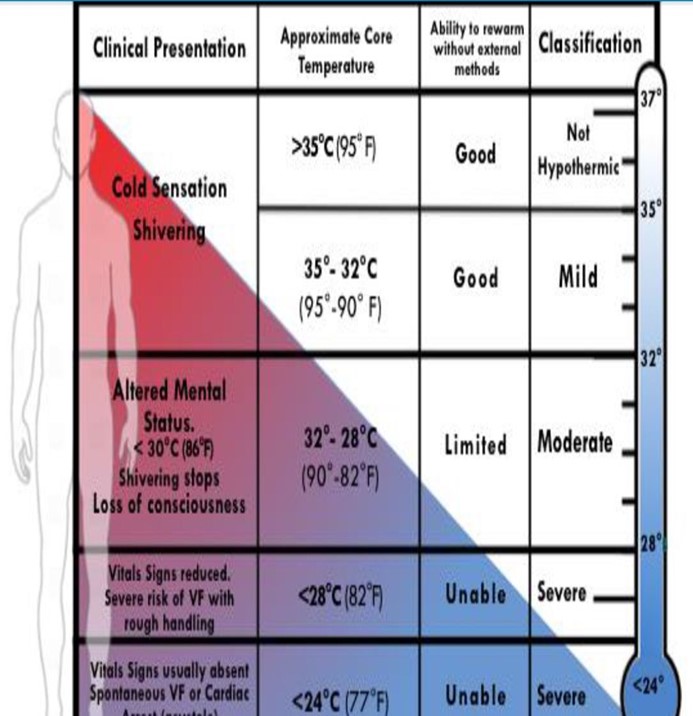
- Classify hypothermia clinically based on vital signs, level of consciousness and intensity of shivering. Core temperature, if available, provides additional information (see chart).
- Handle gently. Maintain the patient in the horizontal position. Continue rewarming during transport. Warm ambulance to 24°C (75.2°F) if possible.
- Prevent further heat loss using insulation and vapour barrier. Move to a warm, sheltered environment. Gently remove (cut off) wet clothing and dry the patient.
- Obtain blood glucose. Support shivering with calorie replacement if alert and able to swallow
- Mildly hypothermic patients should not be allowed to stand or walk for 30 minutes while being kept as warm as possible with calorie replacement and shelter.
- Patients with moderate to severe hypothermia require active external rewarming with chemical, electrical, or forced-air heating packs/blankets. Active rewarming is also beneficial for mild hypothermia.
- Assess the patient for signs of life and pulse carefully for a minimum of 60 seconds to confirm respiratory arrest or cardiac arrest.
- If pulse and breathing are present, continue rewarming techniques.
- If pulse and breathing are absent, start CPR unless contraindications to CPR exist
- Contraindications to CPR in the hypothermic patient include: Obvious signs of irreversible death, chest wall not compressible as whole body is frozen solid, a valid DNR order, avalanche burial > 35 minutes and airway packed with snow, or rescuers exhausted or in danger.
- Rigor mortis or fixed and dilated pupils are NOT a contraindication to CPR in hypothermia.
- Hypothermic patients without contraindications to CPR should have continued CPR and should not be considered for
Termination of Resuscitation (TOR) until the core temperature has been rewarmed to 32°C (90°F) with no ROSC.
- Contraindications to CPR in the hypothermic patient include Obvious signs of irreversible death, chest wall not compressible as the whole body is frozen solid, a valid DNR order, avalanche burial > 35 minutes and airway packed with snow, or rescuers exhausted or in danger
- Transport the patient to the closest appropriate hospital. Patients with prehospital cardiac instability (MAP < 65 (systolic blood pressure < 90 mm Hg) or ventricular arrhythmias, core temperature < 28°C (82°F) and those in cardiac arrest should be transported directly to a center capable of providing a cardiopulmonary bypass (CPB) or extracorporeal membrane oxygenation (ECMO), if feasible.
- CPR may be delayed or given intermittently if necessary to accomplish evacuation.
- Call for AEMT/Paramedic intercept & Assist them in patient care.
AEMT/Paramedic Standing Order
- Establish IV/IO access.
- Administer warm IV 0.9% NaCl 40°C - 42°C (104°F – 107.6°F) in 500 mL boluses.
- Provide airway management as required. With advanced airway, ventilate at half standard rate.
- Administer dextrose IV/IO if hypoglycemic
- Newborn -2 yrs. old Consider Dextrose 25% 4ml/Kg IV/IO Repeat as needed.
- 2 yrs. old Consider Dextrose 50% 2ml/Kg IV/IO Maximum 25gms per dose Repeat as needed.
- Continue CPR if indicated:
- If < 30°C VT or VF or AED advises shock: one shock at maximum power.
- Warm 1 – 2°C or > 30°C prior to additional shocks.
- No vasoactive drugs until 30°C or above. From 30 – 35°C, increase dosing interval to twice as long as normal. Consider epinephrine (1:10,000) (0.1 mg/mL) 1 mg IV/ IO, up to 3 doses.
- Contact Medical Direction for guidance.
Pearls
- A rapid assessment of the patient’score temperature may be performed by placing a warm ungloved hand against the skin of a patient’s back, or chest. If the skin feels warm, hypothermia is unlikely. Hypothermic patients are often significantly dehydrated and may require repeat fluid boluses. Absence of vital signs, rigor mortis, dependent lividity or fixed and dilated pupils may be present in patients with reversible hypothermia and are not a contraindication to CPR. Assume that a hypothermic patient can be resuscitated even if there is an absence of vital signs, any sign of life, rigor mortis, or fixed and dilated pupils.
- Detecting a pulse in a patient with hypothermia may be difficult. Signs of life and pulse should be checked carefully for 60 seconds. Persistent breathing or movement by the patient should prompt a
- strategy of watchful waiting, but if no signs of life are detected, then cardiopulmonary resuscitation (CPR) should be started. Since metabolic needs are so low in severely hypothermic patients, a rate of only a few beats per minute is enough to provide adequate perfusion to vital organs. In such cases, it is better to attempt to maintain effective cardiac activity than to start CPR and cause VF.
- Owing to the decrease in cerebral oxygen requirements with cooling, survival without neurologic impairment may be possible even when it is necessary to perform CPR for hours.
- Immediate continuous CPR is recommended for cardiac arrest due to primary severe hypothermia. Mechanical chest compression devices should be used when available and CPR interruptions avoided. If this is not possible, CPR can be delayed or performed intermittently. Based on available data in a patient with a core
- temperature < 28◦C or unknown with unequivocal hypothermic cardiac arrest, evidence supports alternating 5 min CPR and ≤ 5 min without CPR. With core temperature < 20◦C, current evidence supports alternating 5 min CPR and ≤ 10 min without CPR. If field conditions are not amenable to the safe application of delayed or intermittent CPR, contact Medical Direction to consider Termination of Resuscitation.
- If a patient with cardiac arrest due to hypothermia is rewarmed to a core body temperature that is higher than 32°C and asystole persists, irreversible cardiac arrest is very likely, and termination of CPR should be considered.
- A severely elevated serum potassium level is associated with non-survival and is considered a marker of hypoxia before cooling. Termination of CPR should be considered when the potassium level is higher than 12mmol/L.
- A hypothermic patient should be assessed for coexisting injuries or illnesses that may mimic or conceal the signs and symptoms of hypothermia. The use of vital signs, mental status and presence or absence of shivering may be unreliable if the patient has another condition that coexists with hypothermia. Many conditions such as hypoglycemia, alcohol intoxication and exhaustion can cause altered mental status and can decrease or abolish shivering. A heart rate
- higher than expected for a given level of hypothermia may be due to another cause such as traumatic blood loss.


