Needle Chest Decompression
OBJECTIES:
- Rapidly identify patient with a tension Pneumothorax.
- Properly execute needle insertion and observe for appropriate /desired results.
- Closely monitor the post-intervention patient for recurrence of tension Pneumothorax.
INDICATION
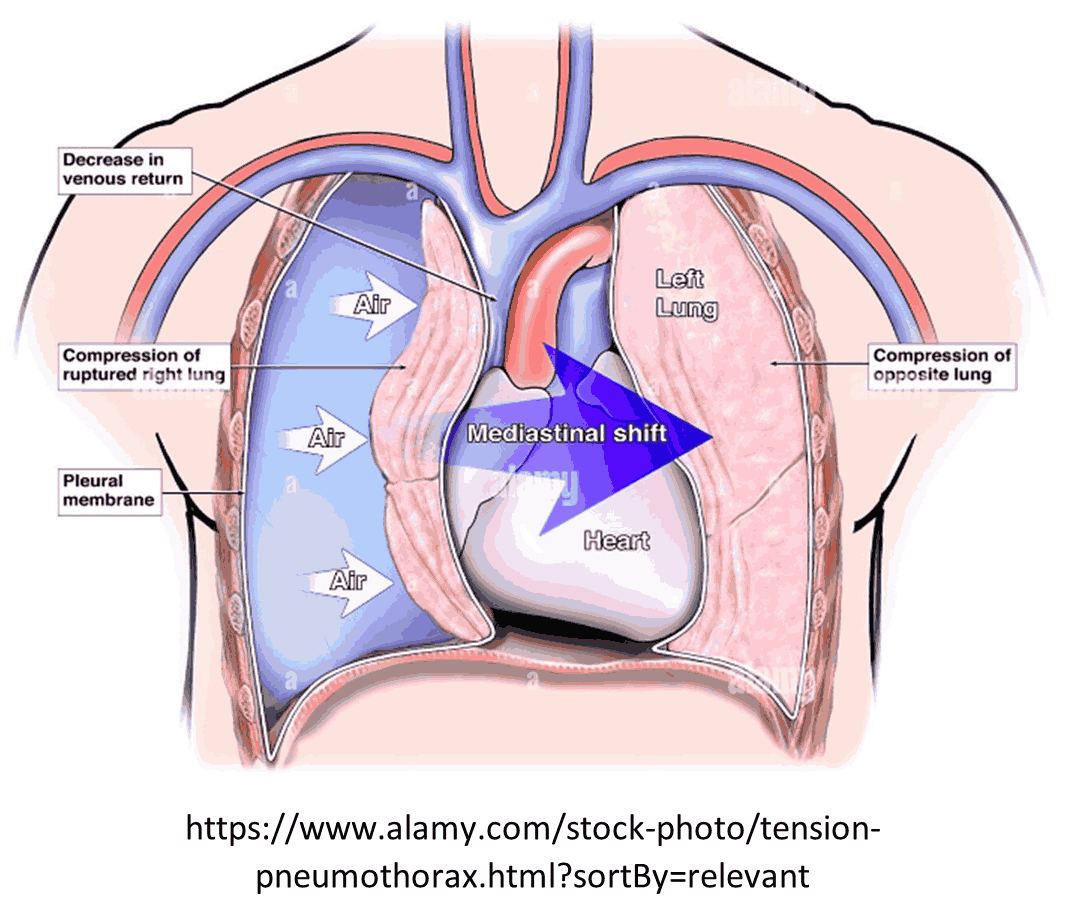
- Patients who are assessed as having an immediate life threat due to tension hemothorax or pneumothorax with absent breath sounds, jugular vein distension, and/or tracheal shift, and evidence of hemodynamic compromise should be rapidly decompressed.
- In addition, needle decompression is indicated in patients who have experienced cardiac arrest secondary to blunt or penetrating trauma.
- Once catheters have been placed in these patients, they should not be removed.
- Any patient with the supportive history and indications of a tension Pneumothorax.
- COPD/other pulmonary pathology with past history of a tension Pneumothorax.
- Patient with multiple /thoracic trauma, with signs of
- Shock.
- Poor/inadequate ventilation.
- Unilateral absent/decreased breath sounds.
- Jugular venous distention.
- Unilateral hyperresonance.
- Tracheal deviation away from affected site.
PROCEDURES
- Maintain ABC; administer oxygen to maintain SaO2 >94%.
- Attach Cardiac Monitor to analyze rhythm obtain BP and Pulse Oxymeter ( SaO2).
- Establish IV/IO access
- Identify patient who will require needle chest decompression.
- Place patient in supine position, if suspected cervical spine injury, stabilize the head and neck. Perform patient assessment, mechanism of injury.
- Prepare the equipment
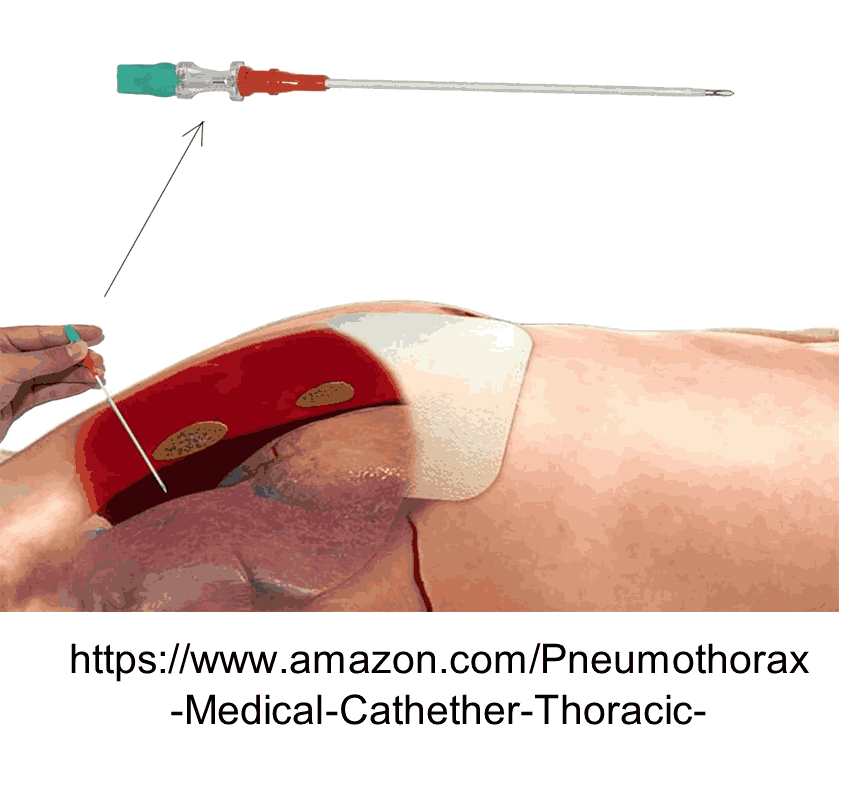
- Size Equipment:-
- Adult 10 - 14 ga. 3-¼” catheter. (catheters for NDT strongly preferred).
- Pediatric 16 - 18 ga. 1½” - 2” catheter.
- Size Equipment:-
- Locate the site:
- Adult
- Lateral site: 4th or 5th intercostal space (ICS) at the anterior axillary line (AAL) preferred,
- Anterior site: 2nd ICS at the mid- clavicular line (MCL).
- Pediatric: 4th ICS at the AAL preferred.
- Adult
- Confirm proper placement site.
- Cleanse insertion site using aseptic technique.
- Insert the needle/catheter unit at a perpendicular angle to the chest wall all the way to the hub, then hold the needle/catheter unit in place for 5 - 10 seconds before removing the needle in order to allow for full decompression of the pleural space to occur.
- Observe for signs of a successful NDC, using specific metrics such as an observed hiss of air escaping from the chest during the NDC process, a decrease in respiratory distress, an increase in hemoglobin oxygen saturation, and/or an improvement in signs of shock that may be present.
- Look for air rush, plunger movement, or aspirated fluid.
- Remove the needle and secure the plastic catheter in place with dressing (do not remove plastic catheter until chest tube is inserted in hospital).
- Assess for ventilation / perfusion improvement, frequently reassess for recurrence of tension pneumothorax.
- Second decompression may need to be performed if there is evidence of reaccumulation, catheter occlusion or dislocation.
MEDICAL DIRECTOR
Contact medical control as soon as possible.
CONTRAINDICATIONS.
- Patients whose tension pneumothorax can be relieved by occlusive dressing management / removal from an open chest wound.
- Patient with suspected simple pneumothorax.
- Patient whose tension pneumothorax can be relieved by the removal of an occlusive dressing from an open chest wound.
COMPLICATIONS
- Intercostal vascular or nerve injury.
- Pneumo/hemothorax.
- Direct damage to the lungs.
- Pericardial /cardiac damage.
- Infection.
PEARLS:-
- Catheter patency should be reassessed during transport, and a second decompression may be needed to maintain ventilatory status if reaccumulation, catheter occlusion, or dislocation occur.
- Anterior axillary line preferred in pediatric population due to anatomic and chest wall thickness differences.
- Any blood aspiration should be noted and recorded to the receiving facility