Orotracheal Intubation
INDICATIONS
Apnea/respiratory failure. Impending respiratory failure. Impaired or absent gag reflex. Only after basic procedures are deemed inappropriate or have proven to be inadequate should more advanced methods be used.
CONTRAINDICATION
- Epiglottitis.
- Facial or neck injuries that prohibit visualization of airway anatomy (relative).
CAUTIONS:
- Pediatric patients should, at least initially, be managed with BVM/SGA.
- Patients with CHF should be managed with trial of CPAP, if possible.
- Avoid intubating patients with severe TBI and asthmatics, if possible.
PROCEDURE:
- Undertake universal precautions.
- Check responsiveness.
- Perform patient assessment and mechanism of injury.
- Maintain neutral alignment of head and neck with cervical stabilization when intubating trauma patients.
- Maximum 2 attempts should be undertaken.
- Limit each attempt to 30 sec.
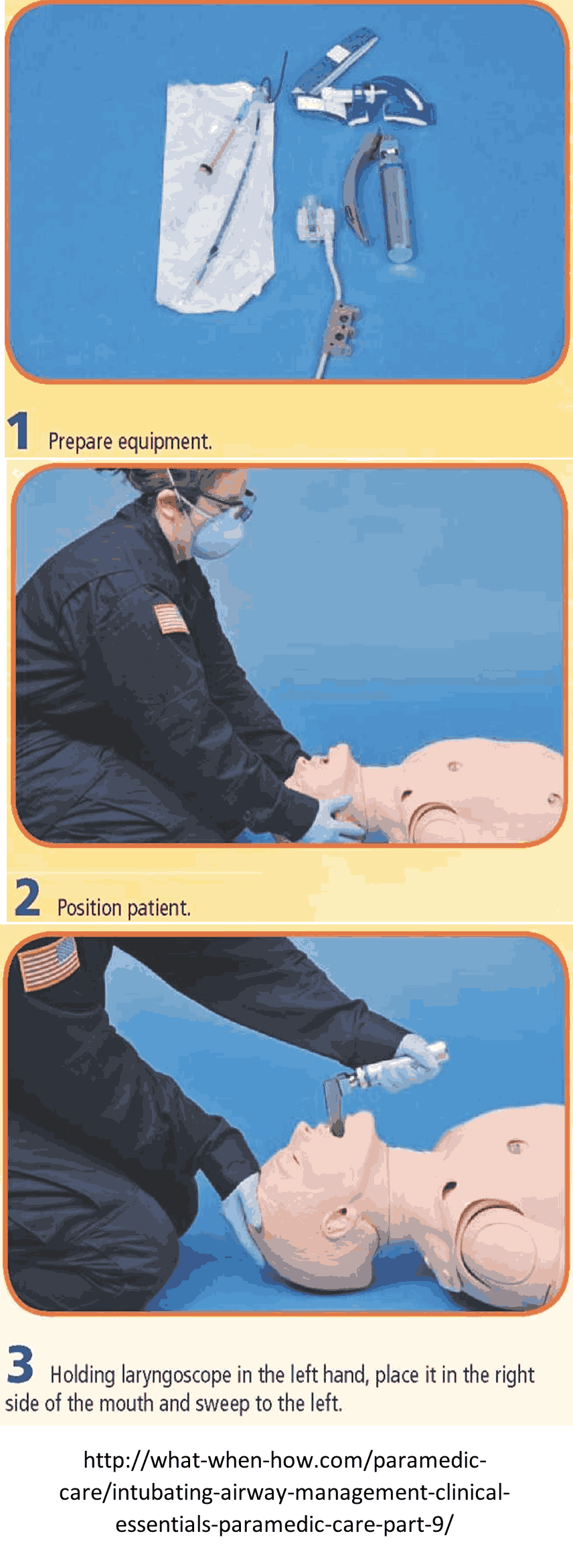
- Prepare all equipment:-
- Endotracheal tube, 10 ml syringe, laryngoscope, blade type and size, style, bag-valve mask, suction device, Magill forceps, water-soluble lubricant, tube holding device or tape and suction device.
- Have suction and Bougie ready.
- Pre-oxygenate the patient with high-concentration oxygen. Three-minute minimum of BVM ventilation or if the patient is breathing, assure 8 vital capacity breaths with NRB. Apply continuous nasal cannula at 15 LPM.
- Place the patient head in a sniffing position with the head hyperextended and neck flexed, if trauma is suspected keep the head and neck in a neutral position.
- Insert the stylet into the ETT, making sure to keep the distal end of the stylet at least 2 cm proximal to the distal tip of the ETT.
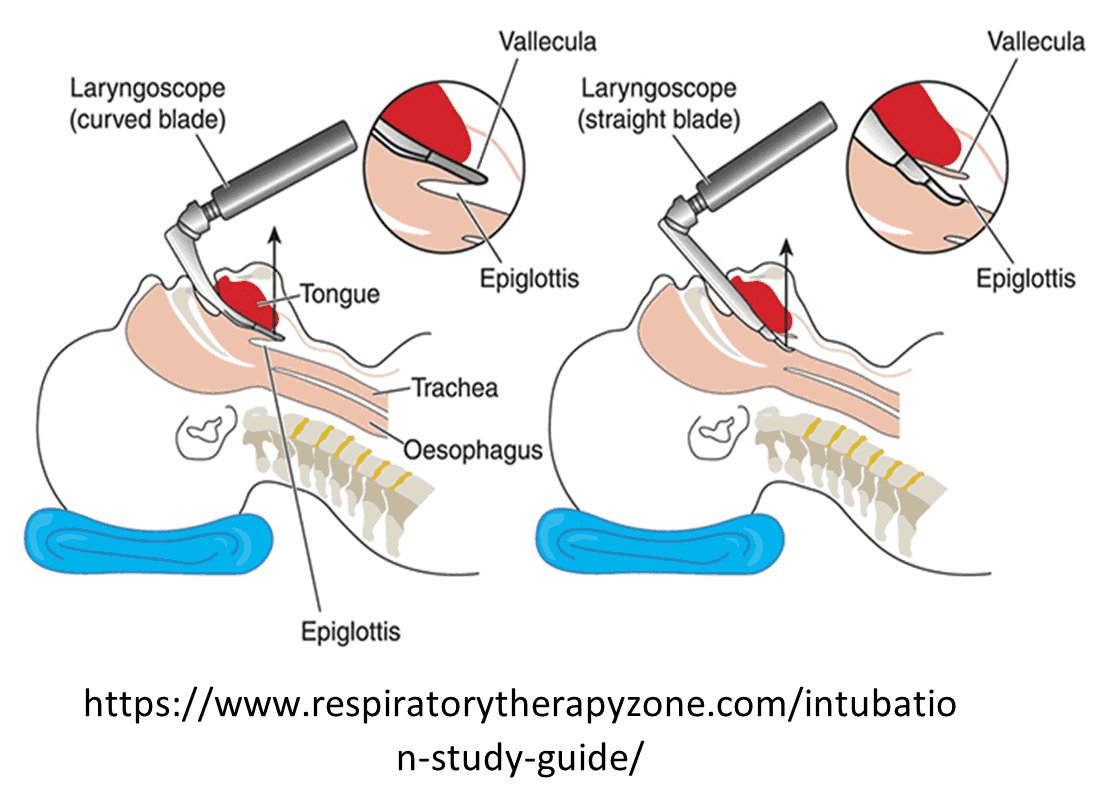
- Open the patient’s airway. While holding the laryngoscope in the left hand, insert the blade into the right side of the patient’s mouth, sweeping the tongue to the left. Use video laryngoscopy, if available and trained.
- Use the blade to lift the tongue and the epiglottis, either directly with the straight (Miller) blade or indirectly with the curved (Macintosh) blade.
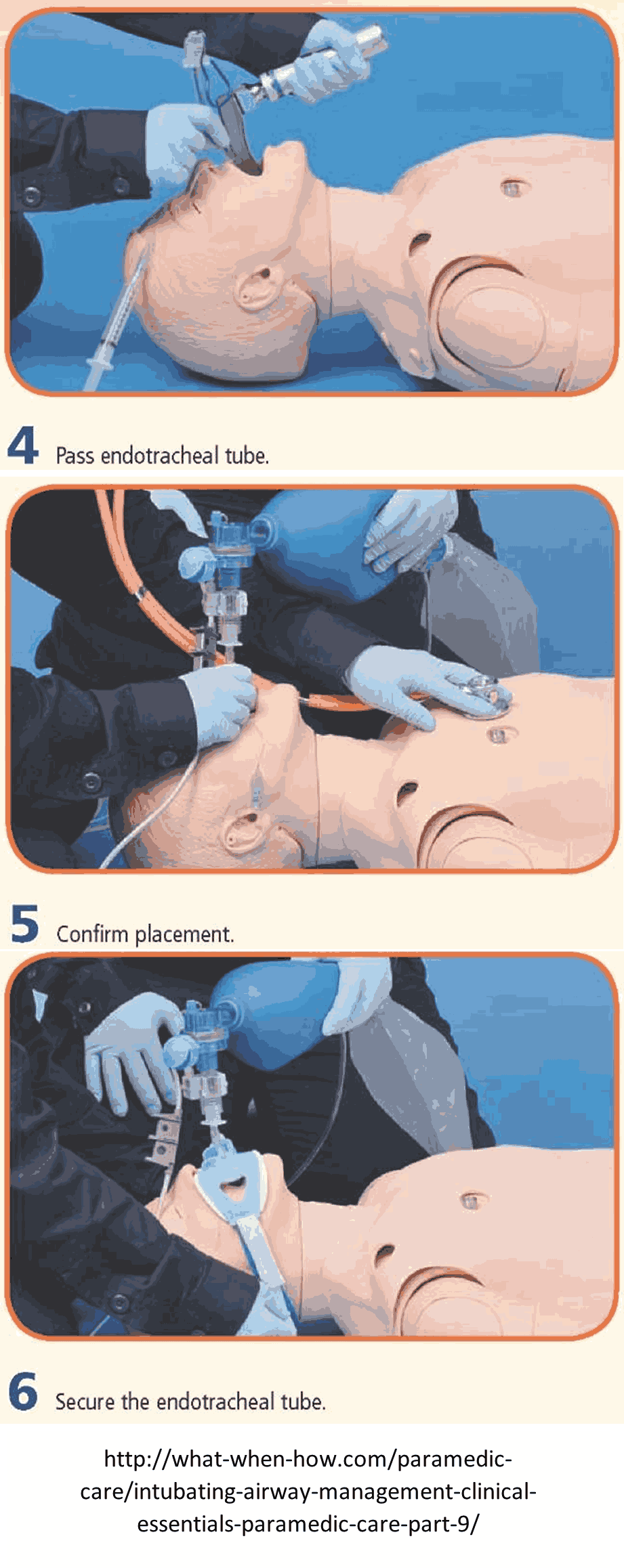
- Once the glottic opening is visualized, insert the tube through the vocal cords and continue to visualize while passing the cuff through the cords.
- Remove the laryngoscope and then the style from the ETT.
- Inflate the cuff with 5 - 10 mL of air.
- Confirm appropriate proper placement with waveform capnography and also document symmetrical chest-wall rise, auscultation of equal breath sounds over the chest and a lack of epigastric sounds with ventilations using bag-valve-mask: -
- Waveform Capnography if available to confirm tube placement and monitor quality of CPR if indicated
- Visualization of the tube passing through vocal cords.
- Chest rise with ventilation.
- Bilateral air entry with auscultation of all lung fields and absence of sound in epigestrium.
- Positive End-tidal CO2 change on an ETCO2 device.
- Presence of condensation inside the ETT.
- Verification of endotracheal placement by esophageal device.
- Documentation of tube depth at the lips.
- Clinical signs of improved perfusion and patient condition.
- Improved oxygen saturation on the pulse oximetry.
- Secure the ETT with a commercial device. Consider applying a cervical collar to minimize head and neck motion during movement and transport.
- Ventilate the patient according to clinical circumstances.
- Bag-valve device.
- Auto. Vent.
- Immobilize the patient head to prevent flexion/extension, and lateral movement with
- Cervical collar.
- Blankets or foam pads.
- Long backboard.
- KED
- Frequently assess tube placement and patient condition.
- Reassess tube placement frequently, especially after the movement of the patient.
- Ongoing monitoring of ETT placement and ventilation status using waveform capnography is required for all patients.
- Document each attempt as a separate procedure so it can be time stamped in the PCR. An attempt is defined as placement of the blade into the patient’s mouth. For each attempt, document the time, provider, placement success, pre-oxygenation, airway grade, ETT size, placement depth, placement landmark (e.g. cm at the patient’s lip), and confirmation of tube placement including chest rise, bilateral, equal breath sounds, absence of epigastric sounds and end-tidal CO 2 readings.
If intubation attempt is unsuccessful, ETT placement cannot be verified or ETT becomes dislodged:
- Remove the tube, monitor oxygen saturation and end-tidal CO2 AND
- Ventilate the patient with 100% oxygen via a BVM until ready to attempt intubation again.
If continued intubation attempts are unsuccessful (maximum of 3 attempts for cardiac arrest) or BVM ventilation is not adequate, consider placing a supraglottic airway. For a viable patient whose airway cannot be successfully managed by any other means, consider Percutaneous Cricothyrotomy Procedure or Surgical Cricothyrotomy
POST INTUBATION CARE
Sedation:
- Fentanyl 50 — 100 mcg (pediatric dose 1 mcg/kg) slow IV/IO push. May repeat every 15 minutes as needed for anesthesia (maximum 300 mcg). AND
- Midazolam 2.5 —5 mg IV/IO (pediatric dose 0.1 mg/kg IV/IO) every 5 — 10 minutes as needed for sedation (maximum 20 mg) OR
- Lorazepam 1 — 2 mg IV/IO (pediatric dose 0.1 mg/kg IV/IO) every 15 minutes as needed (maximum 10 mg).
Contact Medical Direction for additional dosing.
Video-Laryngoscope: If available and trained, use video laryngoscope instead of manual laryngoscope. Video-laryngoscopy has been shown to have better success rates than manual laryngoscopy and should be used if available.
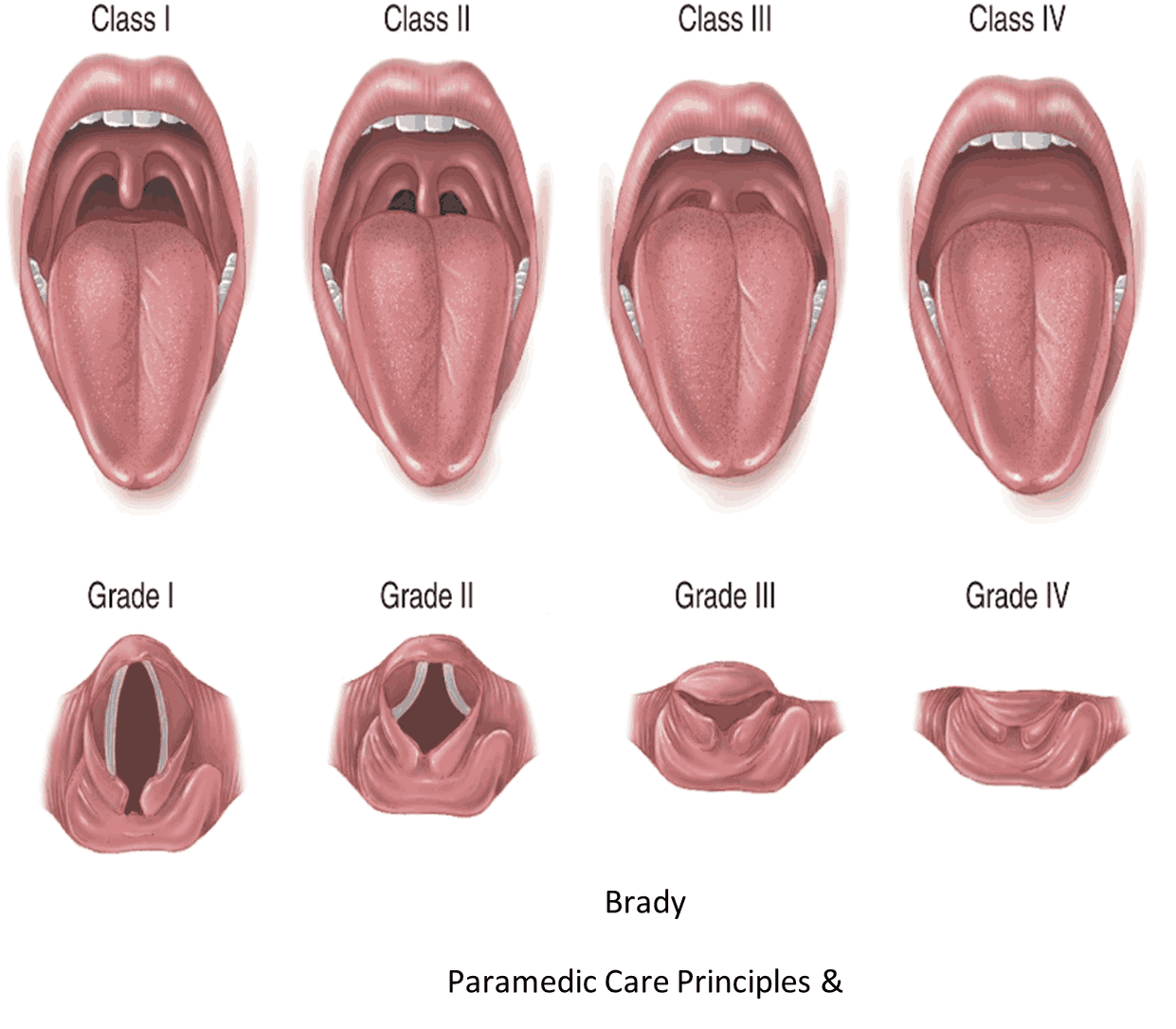
Classifications of Oropharyngeal and Laryngoscopy Views