RESPOND TO SCENE IN A SAFE MANNER
- Review dispatch information.
- Use Incident Command System (ICS) for all responses and scene management.
SCENE ARRIVAL AND SIZE-UP
- Standard precautions, scene safety, environmental hazards assessment, number of patients, need for additional resources, and bystander safety.
- Initiate Mass Casualty Incident (MCI) procedures as necessary.
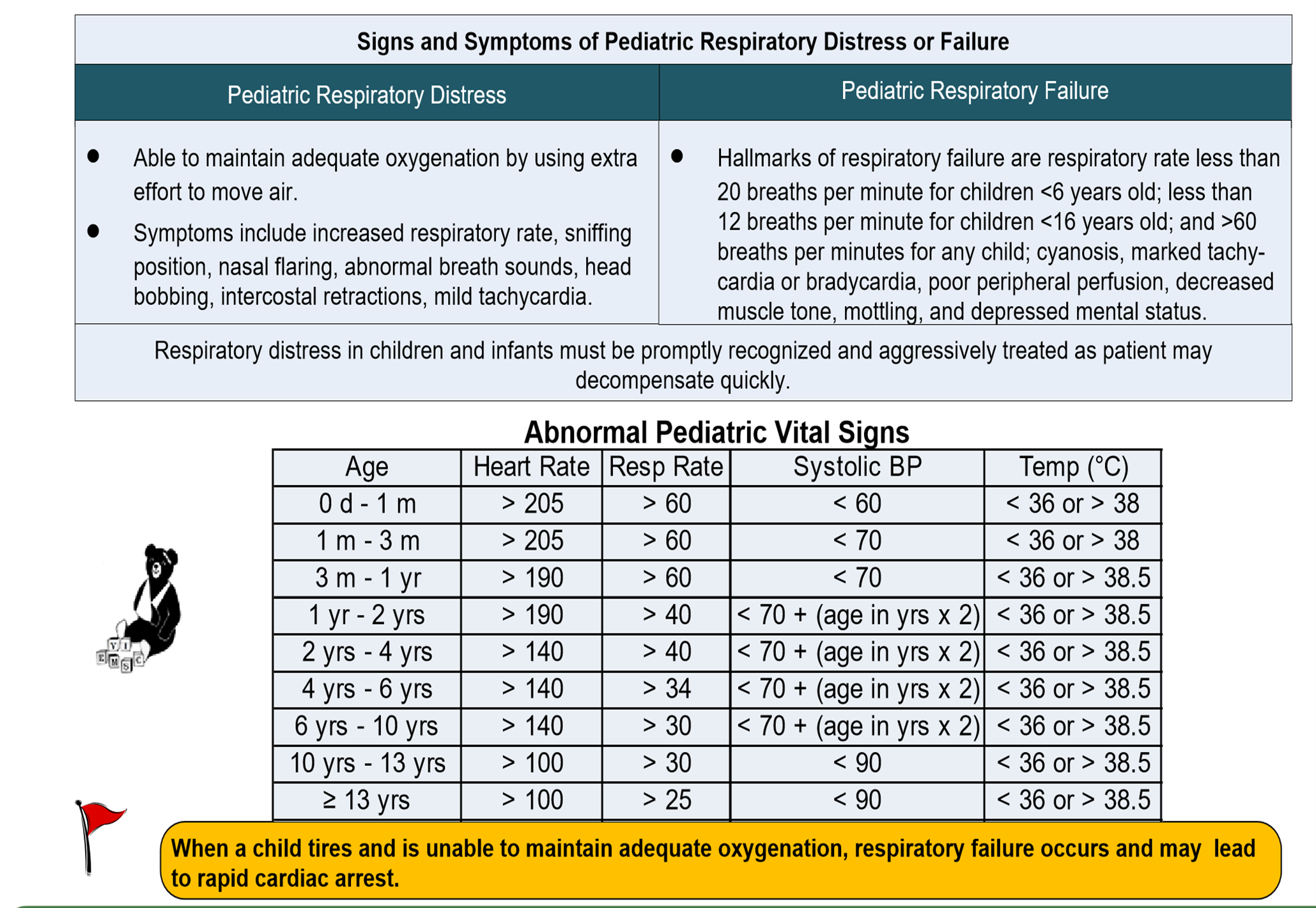
- Call for AEMT/Paramedic intercept, if needed, for patients with unstable vital signs, respiratory distress or other life-threatening conditions.
PATIENT APPROACH
- Determine mechanism of injury / nature of illness.
- If patient is in cardiac arrest, refer to the Cardiac Arrest Protocol - Adult (1 Cardiac) & Pediatric (4 Cardiac).
- Place the Patient in Supine Position or Position of comfort.
- Determine if pediatric protocols apply.
- Establish responsiveness.
- General impression.

| Pediatric Assessment Triangle. | |||
| Appearance | Work of Breathing | Circulation to Skin | |
| Pediatric | Muscle tone, Instructiveness, consolability, Gaze/Look, speech/Cry | Airway Sounds, Body Position, Head bobbing, Chest Wall Retractions, Nasal Flaring, Grunting | Pallor, Mottling, Cyanosis |
Determine if DNR protocol applies.
Primary Assessment
AIRWAY AND BREATHING
- Assess the patient for a patent Airway. If the airway is not patent, take immediate action to correct it (Open & Re Open).
- Assess Breathing:
Breathing Present Yes No Speed Normal Slow Fast Regularity Regular Irregular
- Rate, Effort, Tidal volume, and Breath Sounds.
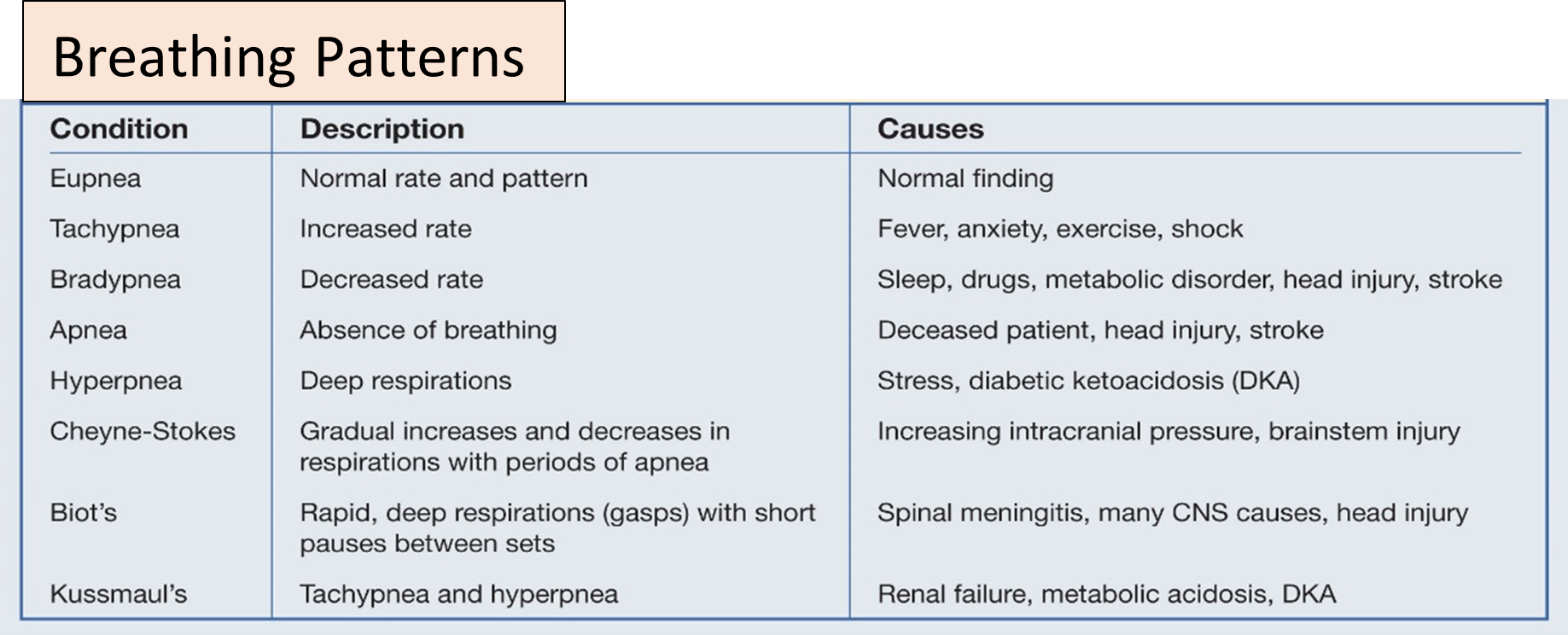
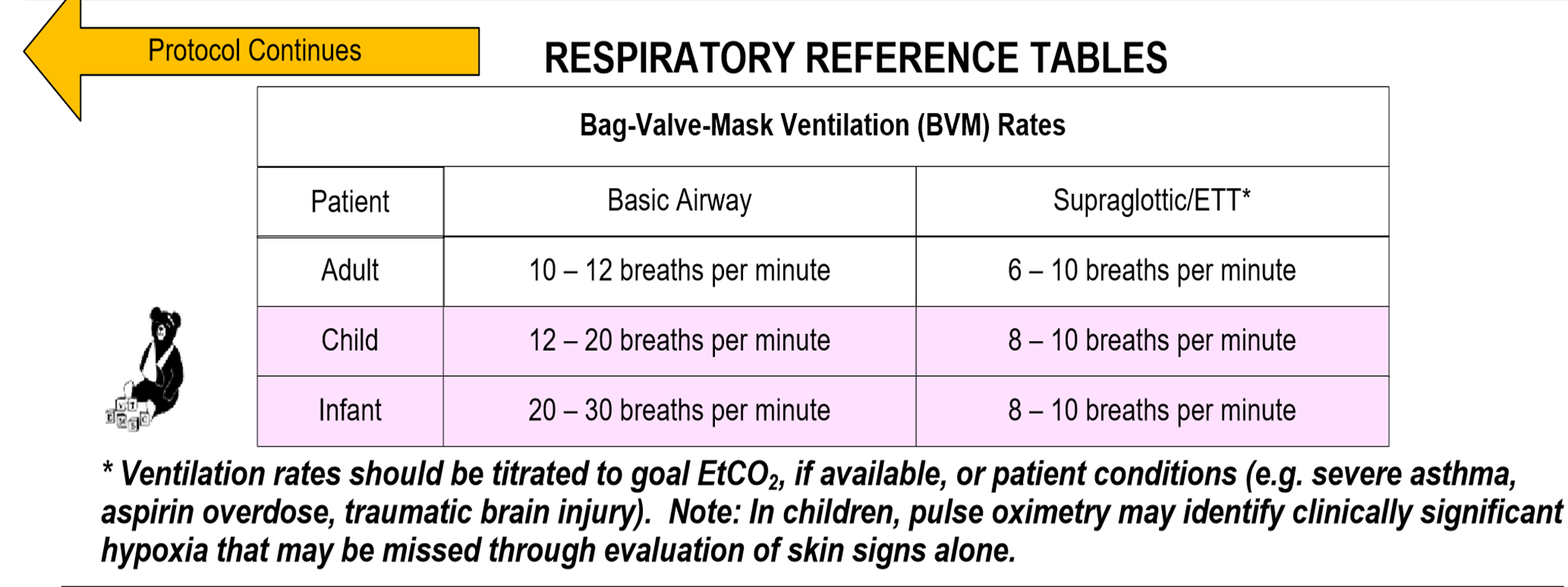
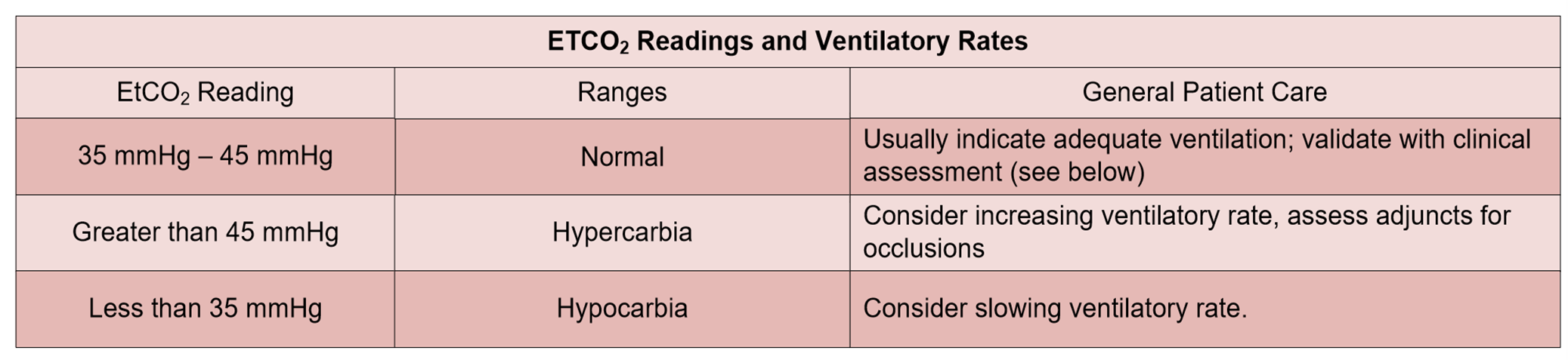
- If breathing is inadequate (slow, shallow), ventilate with 100% oxygen using bag-valve-mask (BVM).
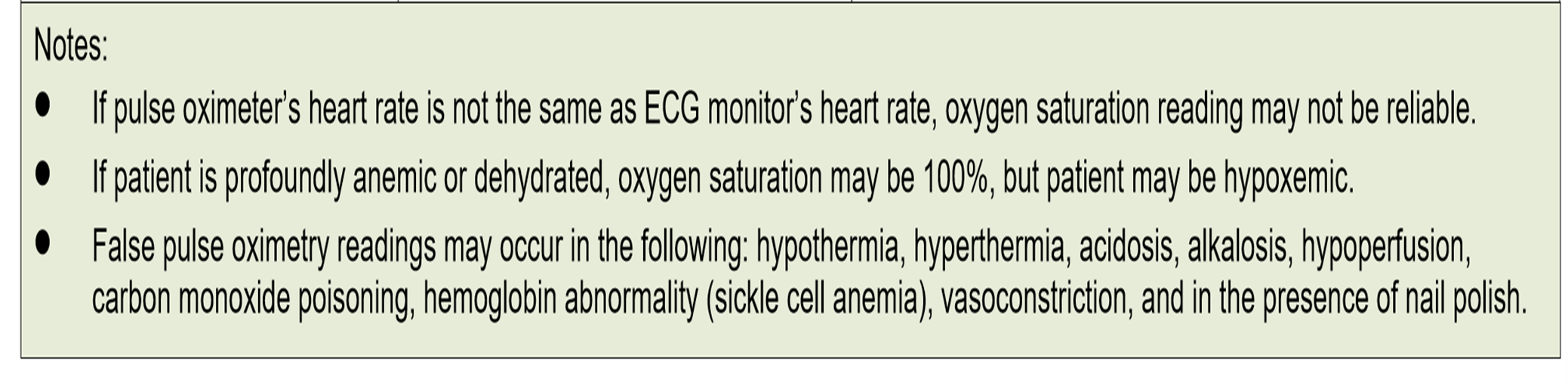
- Administer oxygen as appropriate with a target of achieving 94 % saturation (88 – 92% in COPD). CO- oximetry.
- Assess lung sounds and chest.
- Consider Advance Airway.
CIRCULATION ASSESSMENT
- Assess patient’s
pulse: -
pulse Present Yes No Speed Normal Slow Fast Regularity Regular Irregular
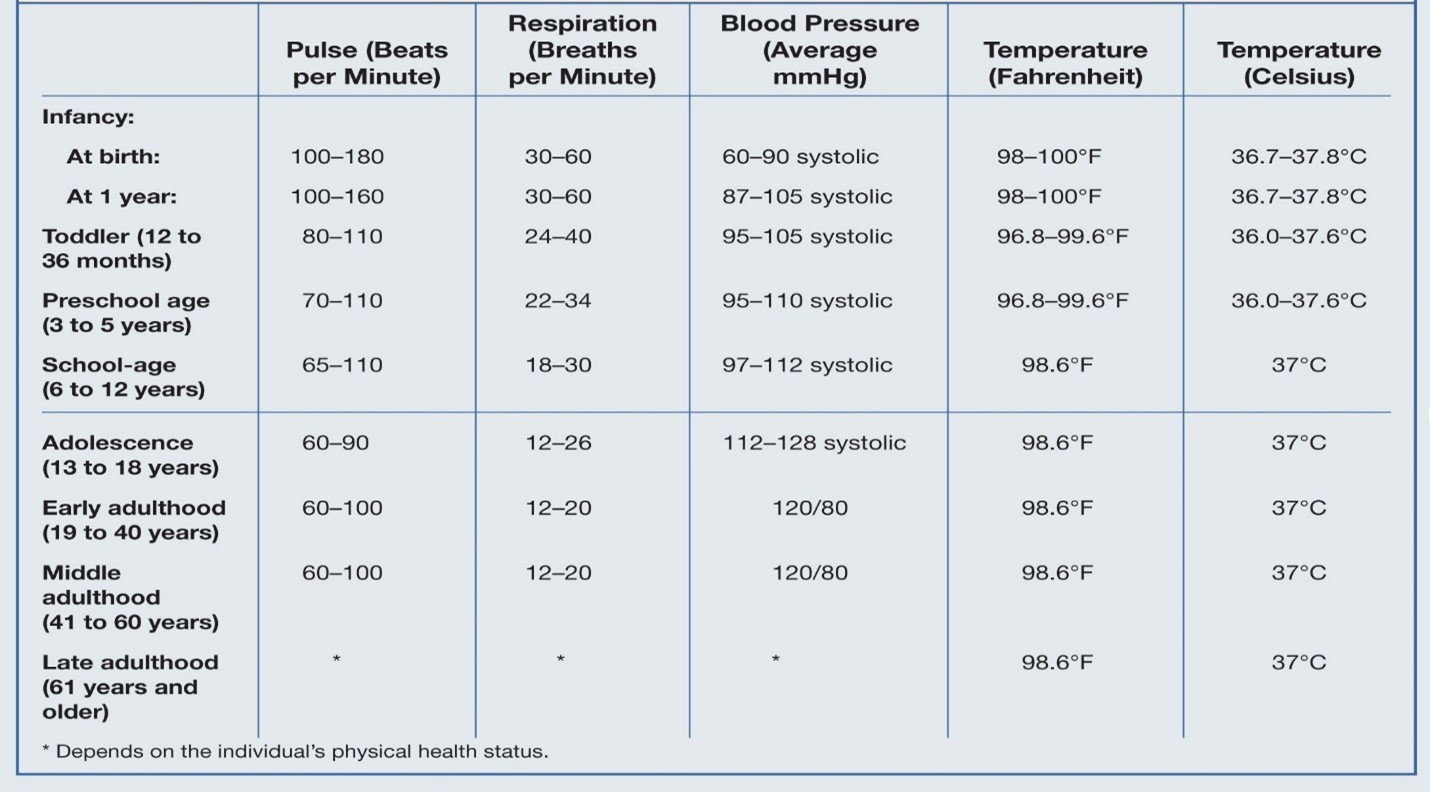
- Check pulse (feel for a pulse for at least 5 seconds but no more than 10 seconds), if no pulse or less than (60 beats/min for pediatric) Start CPR for 2 min, start
- Chest compressions (C-A-B Sequence) (30 compressions: 2 breaths) at a rate at least 100 compressions per minute.
- Assess patient’s Skin: -
| Skin | |||
| Tem | Warm | Hot | Cold |
| Color | Pink | Yellow | Red |
| Condition | Dry | Moist | |
- Assess patient’s Capillary Refill Time for pediatric: - (2 –seconds).
- Control bleedingusing direct pressure, pressure bandages, tourniquets.
- Establish IV access
and fluid resuscitation as appropriate for the patient’s
condition.
- For adult patients, administer fluids to maintain systolic blood
pressure refer to Shock Protocol – Adult (56 Medical).
- For pediatric patients, administer fluids based on physiological signs and therapeutic end-points refer to Shock Protocol – Pediatric (60 Medical).
- For adult patients, administer fluids to maintain systolic blood
pressure refer to Shock Protocol – Adult (56 Medical).
DISABILITY ASSESSMENT
- Assess level of consciousness appropriate for age; use (AVPU) Scale.
- If altered level of consciousness, check blood glucose.
- Utilize spinal motion restriction if indicated by assessment, see Advanced Spinal Assessment Procedure and Policy for Ault & Pediatric refer to Spinal Immobilization protocol (55 skills).
EXPOSE ASSESSMENT
- Remove the patient's cloths and take care of privacy.
TRANSPORT DECISION
- All patients should be transported to the closest appropriate Health Institutions (Hospital, Polyclinic, and Health Center).
- Regionalized systems of care for specialized trauma patients may necessitate transport to specialized center (Trauma, Burn Center).
- Notify receiving facility.
- Consider aeromedical transportation when indicated.
Secondary Assessment
SECONDARY/FOCUSED ASSESSMENT AND TREATMENT
- Reassess chief complaint, history of present illness.
- Complete a physical assessment as appropriate for the patient’s presentation.
| Trauma Patients | MOI | Ph/Exam (DCAPBTLS) | |
| Medical Patients | chief complaint, history of present illness | SAMPLE History |
Pain Assessment (OPQRST) (0 – 10) Scale. |
- Consider field diagnostic tests including: attach cardiac monitoring, obtain 3/12-lead ECG, blood glucose, body temperature, stroke assessment, pulse oximetry, etc.
- Check Pupil for light reaction.

Take full set of vital signs. (it is the base set of vital signs).
- Check disability by using Glasgow Come Scale.
-
Adult Glasgow Coma Scale
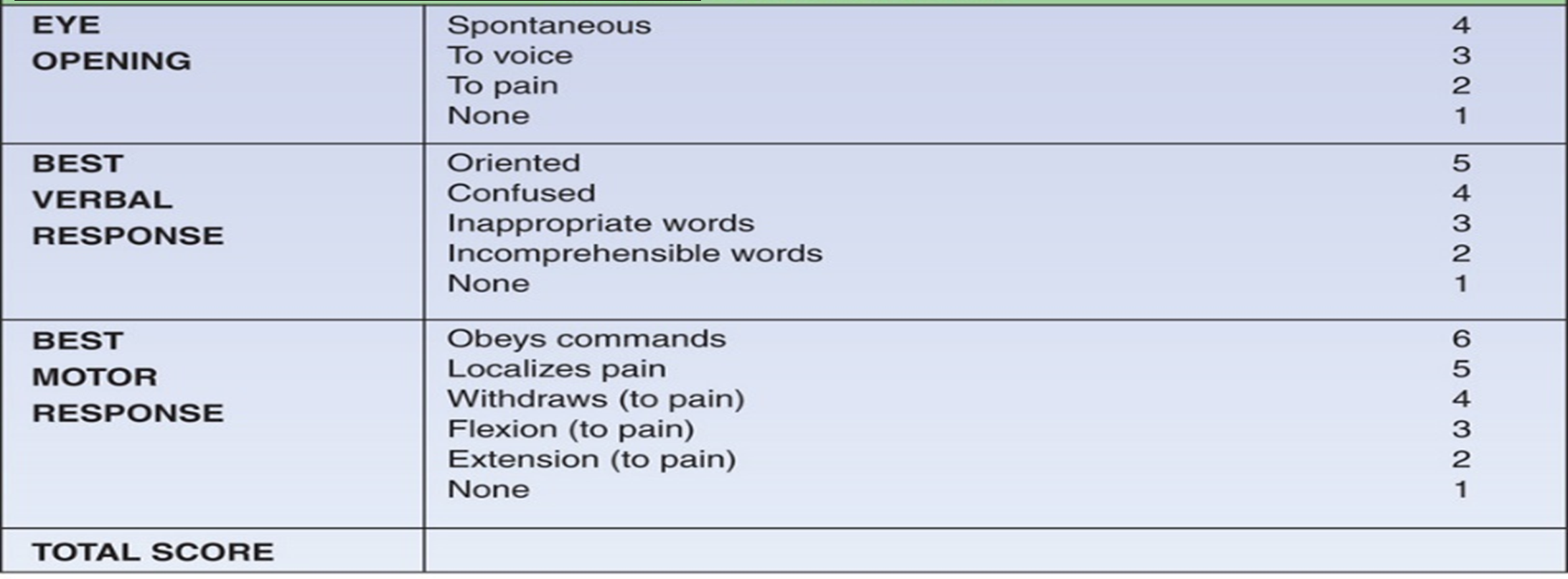
-
Pediatric Glasgow
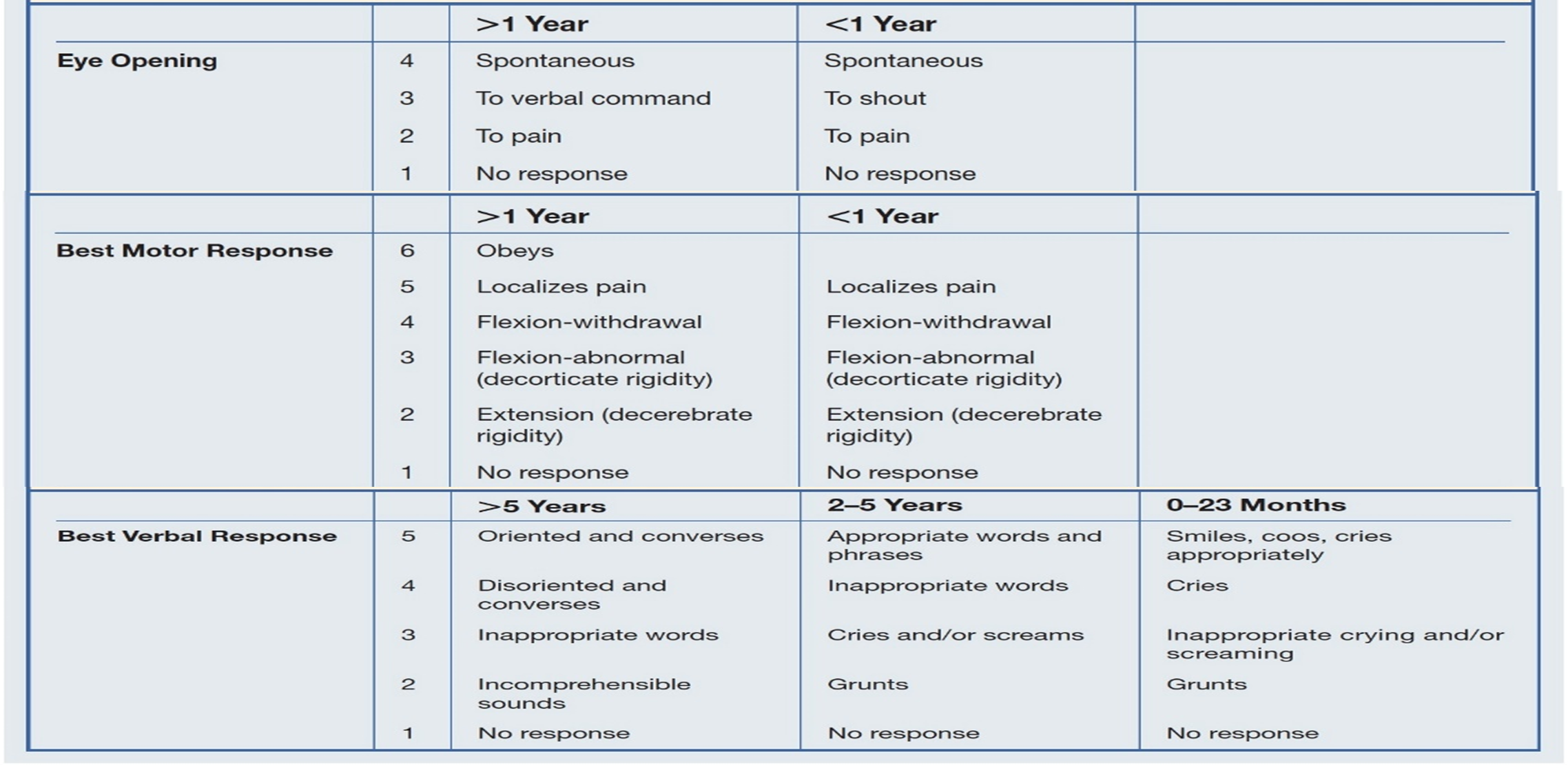
- Refer to appropriate protocol(s) for further treatment options.
- Dress and bandage lacerations and abrasions.
- Cover evisceration with a sterile dressing to prevent heat loss.
- Maintain normal body temperature.
- Stabilize impaled objects. Do not remove an impaled object unless it interferes with CPR or your ability to maintain the patient’s airway.
- Recheck vital signs at least every 15 minutes (for stable patient) and at least every 5 minutes (for unstable patient).
TRAUMA SYSTEM
See Traumatic Emergencies Protocol (1 Trauma).