SPINAL IMMOBILIZATION
OBJECTIVES
- Identify patient with spinal injury.
- Select the appropriate type and size of spinal immobilization.
- Rapidly apply spinal immobilization.
INDICATION OF PROCEDURE
- Trauma patient e.g. RTA, fall, gunshot or stab injury near the spine.
- Medical patient with suspected spinal injury.
STANDING ORDERS:-
- Routine Patient Care.
- Perform advanced spinal assessment to determine if patient requires spinal motion restriction.
- Maintain manual in-line stabilization during assessment, unless patient is alert and spontaneously moving neck.
- Minimize spinal movement during assessment and extrication.
- A long backboard, scoop stretcher, vacuum mattress, or other appropriate full length extrication device may be used for extrication if needed. Do not use short board or KED device, except for vertical extrication or other special situations.
- Apply adequate padding to prevent tissue ischemia and minimize discomfort.
PROCEDURE
- Undertake universal precautions.
- Note the mechanism of injury.
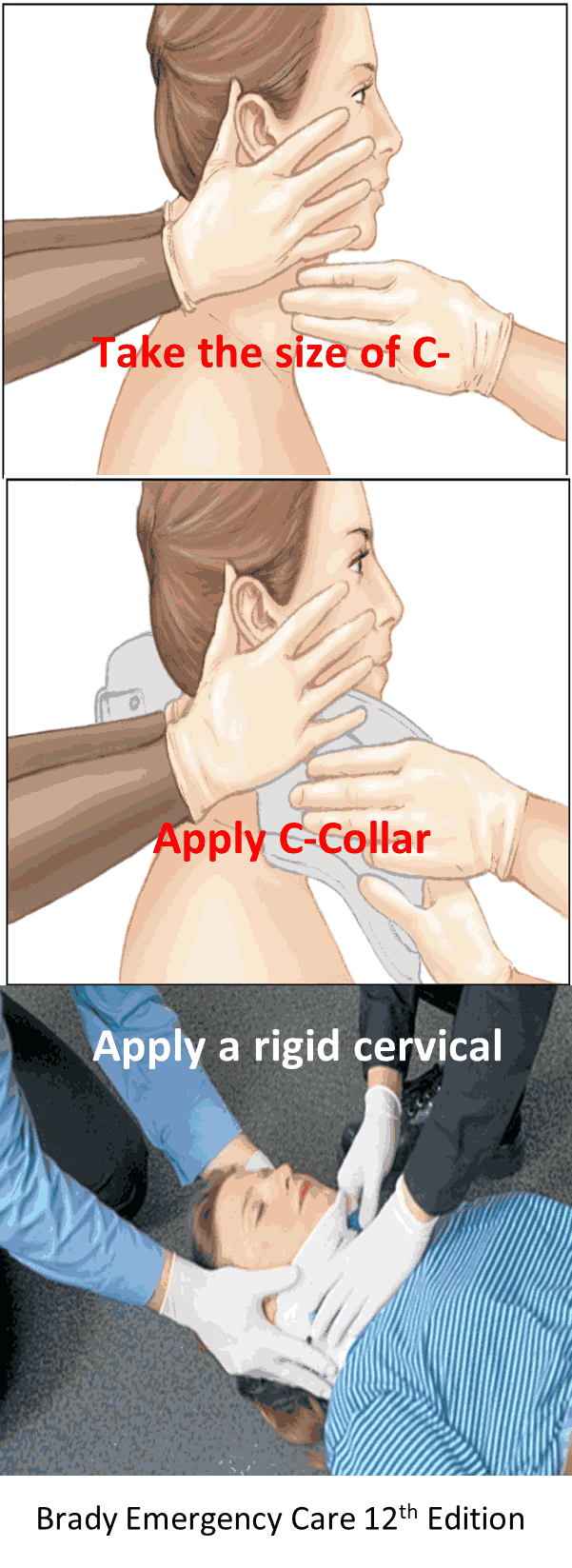
- Apply a rigid cervical collar.
- Maintain ABC, administer oxygen if needed Maintain SPO2>94%.
- Perform Patient assessment (history, mechanism of injury, medications, past history and allergies).
- The patient can be transported without C-spine immobilization if the EMT verify the absence of any of the
following
findings.
- Neck pain.
- Distracting injuries.
- Medications, drugs or alcohol that may mask the perception of pain.
- Altered level of consciousness.
- Tenderness on palpation of the neck and shoulders.
- Pain while shurging the shoulders.
- Pain on active full range of movement of the head.
- Significant language barrier.
- Parasthesia/Dysasthesia or any unexplained neurological sign and symptoms.
- If any doubt exists e.g. significant mechanism of injury, then patient should be fully immobilized with c-spine and long spine board.
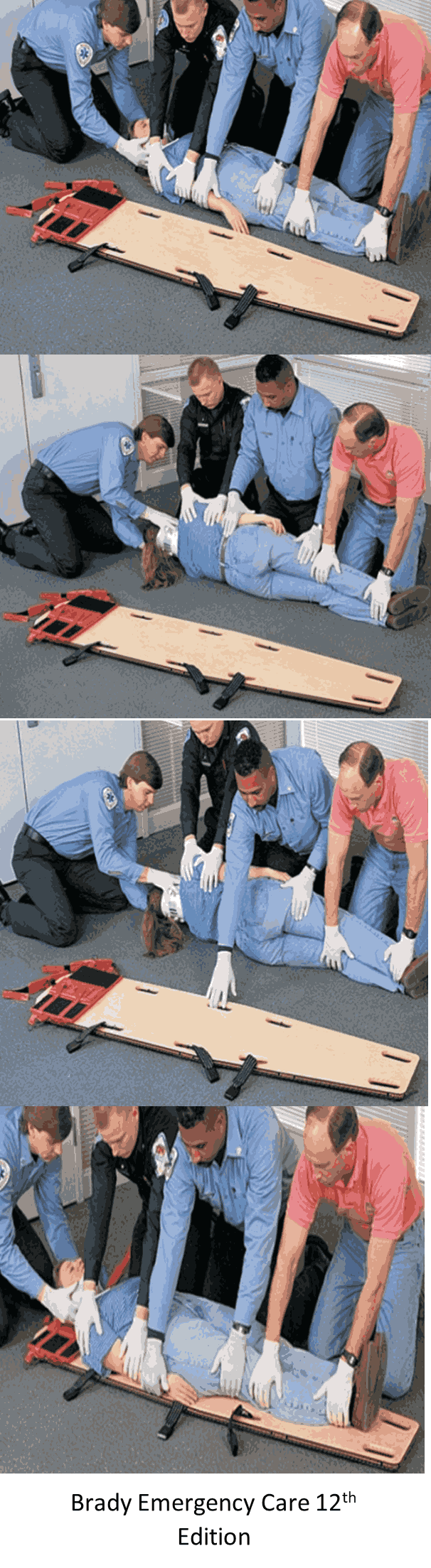
- Rescuer one should keep the head and neck in neutral position throughout the procedure.
- The second rescuer will perform physical assessment including PMS.
- The second rescuer measures and applies cervical collar.
- Place the patient with legs extended, one arm (uninjured) will be placed extended underneath the body when the patient is rolled on their side, the other arm is placed by the patient’s body.
- The long board is placed next to the patient, if one arm is injured, place the board next to the injured side, this will force the patient to be rolled onto his/her uninjured side.
- The second rescuer will kneel in position next to the patient’s chest; one hand should be placed on the patient’s shoulder, the other hand placed on the patient’s flank.
- The third rescuer will kneel in position next to the patient’s thigh, one hand placed on the patient’s hand and hip, the other placed on the patient’s leg, by the knee.
- Both rescuers should be positioned directly opposite the long spine board.
- The first rescuer will give orders to roll the patient as a unit onto his/her side towards the second and third rescuers while he/she maintain the head and neck in neutral position.
- While the patient is on his/her side, the patient back, buttocks and legs are inspected for injuries.
- The long board is slide into place by the second and third rescuers, patient rolled back and repositioned
correctlyon the board by sliding him downward then upward to the
center of the backboard and latter secured
- Beginning at the ankle, secure the patient respectively to the long spine board at
- Knees.
- Hips.
- Chest.
- Shoulders. secure the patient head to the long board by strapping two blanket rolls or other devices on each side of the patient’s head to the long board.
- Reassess PMS in each extremity after securing the patient to the device.
Apply padding underneath the patient’s body if necessary.
- Beginning at the ankle, secure the patient respectively to the long spine board at
- In situations requiring rapid extraction (refer to rapid extraction protocol).
- Self-extrication by patient is allowable if patient is capable.
- Allow ambulatory patients to sit on stretcher and then lie flat. (The "standing take-down" is eliminated.)
- Position backboarded patient on stretcher then remove backboard by using log roll or liftand-slide technique.
- Situations or treatment priorities may require patient to remain on backboard, including the multi-trauma patient, combative patient, elevated intracranial pressure.
- Head immobilization may be appropriate for patients unable to control their own movements.
- With the patient lying flat, secure patient firmly with all stretcher straps and leave the cervical collar in place. Instruct the patient to avoid moving head or neck as much as possible.
- Elevate stretcher back only if necessary for patient compliance, respiratory function, or other significant treatment priority.
- If patient poorly tolerates collar (e.g., due to anxiety, shortness of breath, torticollis), replace with towel roll and/or padding.
- Patients with nausea or vomiting may be placed in a lateral recumbent position. Maintain neutral head position with manual stabilization, padding/pillows, and/or the patient's arm.
- Patient may remain in own safety seat after motor vehicle crash if it has a self-contained harness with a high back and two belt paths and is undamaged. If all criteria are not met, use ambulance’s safety seat.
- If the patient requires significant care (e.g. airway management) that cannot be adequately performed in a car seat, remove the patient and secure him/her directly to the stretcher.
Pediatric Patients
Requiring a Child Safety Seat
- For pediatric patients requiring spinal motion restriction, transport in a child safety seat per.
- Apply padding and cervical collar as tolerated to minimize the motion of the child’s spine.
- Rolled towels may be used for very young children or those who do not tolerate a collar.
MEDICAL DIRECTOR:-
(Contact medical director as soon as possible.).
- Patients with only penetrating trauma do not require spinal motion restriction.
- Caution should be exercised in older patients (e.g., 65 years or older) and in very young patients (e.g., less than 3 years of age), as spinal assessment may be less sensitive in discerning spinal fractures in these populations.


