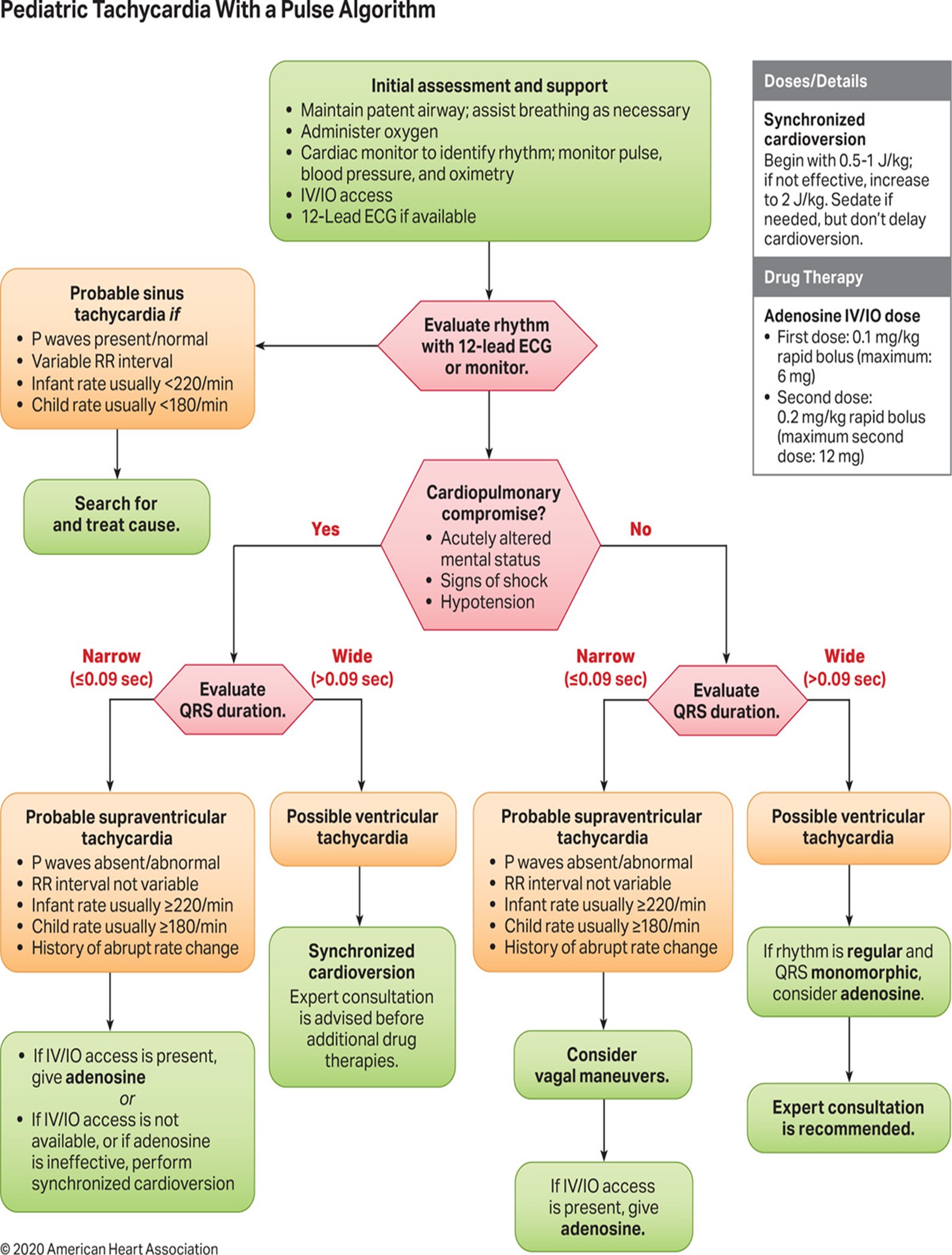
Tachycardia - Pediatric
EMT STANDING ORDERS:
- Routine Patient Care
- If serious signs or symptoms (hypotension, acutely altered mental status, signs of shock, ischemic chest discomfort, or acute heart failure); Call for Paramedic intercept, if available.
- Obtain 3 lead ECG if available.
- Establish IV access to KVO.
- Call for AEMT/Paramedic intercept. & Assisst AEMT/Paramedic in patient care.
AEMT/PARAMEDIC STANDING ORDER:
- Follow PALS guidelines as trained and credentialed.
If symptomatic and hemodynamically unstable:
- For narrow complex/probable SVT:
- Adenosine 0.1 mg/kg rapid IV/IO not to exceed 6 mg (first dose), followed by a rapid flush. Repeat once at 0.2 mg/kg not to exceed 12 mg.
- If adenosine is ineffective or for wide complex, perform synchronized cardioversion: 0.5 - 1J/kg; if unsuccessful, increase to 2J/kg. (Refers to per protocol).
- For narrow complex/probable SVT:
- If symptomatic but hemodynamically stable:
- For narrow complex: probable Supraventricular Tachycardia, or regular wide complex tachycardia (monomorphic QRS ONLY): Adenosine 0.1 mg/kg IV/IO not to exceed 6mg (first dose). May repeat once at 0.2 mg/kg IV/IO not to exceed 12 mg (subsequent dose).
- For wide complex: Amiodarone 5 mg/kg IV/IO (maximum 300 mg) over 20-60 minutes OR Procainamide 15mg/kg over 30 to 60 minutes. Seek expert consultation.
- For polymorphic ventricular tachycardia/Torsade de Pointes: Magnesium sulfate 25 - 50 mg/kg IV/IO over 10 - 20 minutes (maximum dose 2 grams).
- Consider expert consultation.