Traumatic Cardiac Arrest (TCA) (Adult & Pediatric)
EMT Standing Orders:
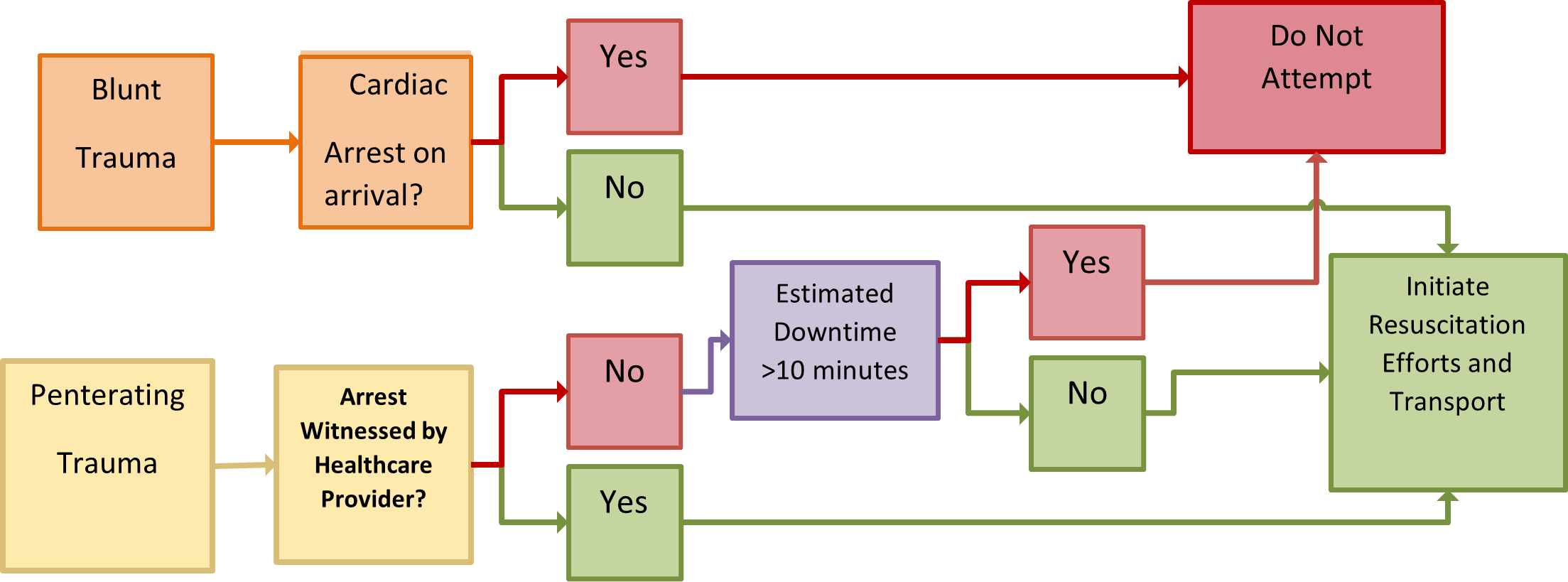
- Determine if resuscitation is indicated per the above flowchart. If resuscitation is initiated, transport immediately and limit scene time to < 10 minutes (if possible).
- Routine Patient Care with a focus on continuous manual chest compressions and AED use.
- Ventilate with BVM, 1 breath every 6 seconds.
- Provide early airway intervention using oral and/or nasal airways and suction
- Control internal and external hemorrhage.
- See Traumatic Emergencies Protocol and Tourniquet & Hemostatic Agent Protocol - Adult & Pediatric.
- Apply pelvic binder as indicated as you train.
- Align long bone fractures, and splint as indicated.
- Attempt to maintain spinal motion restriction by minimizing head movement. Do not apply a cervical collar before ROSC.
- If ROSC occurs, see Post Resuscitative Care Protocol - Adult or Pediatric.
- See Trauma Triage and Transport Decision Policy.
- Consider activation of Air Medical Transport Call for AEMT/Paramedic intercept. & Assisst AEMT/Paramedic in patient care.
- Alert receiving facility of a trauma alert and a patient in cardiac arrest
- Consider not initiating resuscitation or early termination of efforts if there are obvious signs of death, injuries that are not compatible with life, or if there has been a prolonged downtime. See Resuscitation Initiation and Termination.
AEMT Standing Orders - ADULT:
- Place IV/IO without interrupting chest compressions
- Administer 500 mL - 1000 mL of 0.9% NaCl, repeat as needed. Warmed fluids should be used where available to aid in shock treatment.
- Epinephrine is NOT recommended in traumatic cardiac arrest.
- Consider the placement of the supraglottic airway and ensure the quality of ventilation with waveform capnography.
AEMT Standing Orders - PEDIATRIC:
- Administer fluid bolus 20mL/kg of 0.9% NaCl by syringe method (may repeat to a maximum of 60 mL/kg). Warmed fluids should be used where available to aid in shock treatment.
- Consider the placement of supgraglottic airway and ensure the quality of ventilation with waveform capnography.
PARAMEDIC STANDING ORDERS:
- Consider early placement of an endotracheal tube without interrupting chest compression. See Airway Management Procedure, Orotracheal Intubation Procedure, or Percutaneous Cricothyrotomy Procedure.
- Consider leaving supraglottic airway in place, if effective. Monitor placement with capnography.
- Perform bilateral needle chest decompression. See Thoracic and Abdominal Injuries Protocol and Needle Decompression Thoracostomy (NDT) Procedure.
- If Return of Spontaneous Circulation (ROSC) occurs, consider tranexamic acid. (See Tranexamic Acid (TXA) Protocol).
- Epinephrine and antidysrhythmics are not recommended in traumatic cardiac arrest.
- Apply cardiac monitor and treat displayed rhythm. Confirm with point-of-care ultrasound, if available and trained.
- Asystole or PEA with a rate < 40.
- Terminate Resuscitation See Resuscitation Initiation and Termination.
- PEA with rate > 40.
- Rapid transport to nearest appropriate facility, with ongoing resuscitation
- VFib / VTach.
- Defibrillate, and initiate rapid transport to the nearest facility, with ongoing resuscitation.
PEARLS:
- Use warmed fluids when administering fluid bolus to patients in TCA, as shock management is crucial in this population.
- It has been identified that cardiac arrest as a result of blunt force trauma has an almost 100% mortality rate. Cardiac arrest from penetrating trauma has a higher likelihood of survivability with recent advancements in trauma care.
- Due to the nature of traumatic cardiac arrest, patients may not always strictly meet the criteria for TOR. This protocol is designed to be a decision making guide: if in doubt, start resuscitation and follow established protocols.
- Always remember, a medical cardiac arrest can lead to a traumatic injury (e.g., a cardiac arrest while driving).


